From Alliance Magazine—
Editor’s Note: The following is an excerpt of an article that appears in the Summer 2020 Edition of Alliance Magazine, published by the Muncie-Delaware County Economic Development Alliance. A PDF of the entire article and full Summer 2020 Edition of the magazine can be viewed at the link at the very bottom of this article.
Muncie, IN—Hospitals and clinical practices around the globe have been rocked by the COVID-19 pandemic. Those that haven’t been inundated by those actually suffering from the virus have been hit with a mammoth new reality: personal visits are out for the most part, while telemedicine is emerging as the sole alternative to building-based healthcare delivery. According to an article in the April 2020 edition of the medical journal The Lancet, physicians in China’s Wuhan province, where COVID-19 emerged, urged infected patients to contact care providers online.
That practice served as a model for other countries who began seeing a surge in infected citizens. Today, virtualized approaches to medicine are ubiquitous in the face of a pandemic that has millions abiding by stay-at-home and social distancing orders. No one, least of all healthcare delivery workers, wants to get infected, and that reality is driving so-called telehealth.
Eric Tharp, Vice President, Chief Practice Officer for IU Health’s East Central Region, said telemedicine and virtual healthcare visits are a rapidly growing segment in his region. He said IU Health is utilizing expanded federal rules regarding telemedicine to help stay connected to patients and provide them with some peace of mind during an uncertain time.
Tharp said while much of the equipment necessary for a higher volume of telehealth visits was already in place, the training for physicians and education for patients on how to use the technology is still ongoing.
“We have increased our time investment for sure,” Tharp said in regard to its growing telehealth strategies. “Patients already know what to expect with an in-person physician visit. But, they may have never experienced a virtual visit before. They might need help trying to open links they’ve been provided. There are definitely different challenges for different patients. We’ve spent a lot of time getting patients educated on how they’ll be contacted and the technology associated with that. We’re also working to help physicians understand some of these things.
A major factor in telehealth’s rapid, virus-driven growth was a move by the federal Centers for Medicare and Medicaid Services (CMS) to dramatically ease restrictions relating to virtual healthcare delivery.
According to The Lancet, in late March, CMS officials announced an “an unprecedented array of temporary regulatory waivers and new rules to equip the American healthcare system with maximum flexibility” to respond to the pandemic.
Tharp said one such regulation change now allows physicians in one state to conduct telehealth visits with patients across state lines, something strictly prohibited in the pre-pandemic rule book.
While it seems telehealth has successfully bridged the gap between doctor and patient, there are, of course, drawbacks. The most obvious, Tharp said, is the physical component. “We can’t do physical exams, and that means we can’t use our instruments to help determine a patient’s health,” said Tharp. “For example, we are unable to look into a patient’s throat or into a patient’s ears. We can’t listen to their heartbeat. There are definitely limits to what telehealth can do. But, it’s still important that we’re able to offer our patients some assurances. That’s why routine checkups, even if they’re done virtually, allows us to buy some time until we feel like we really need to see that patient in person.”
—End of excerpt.—
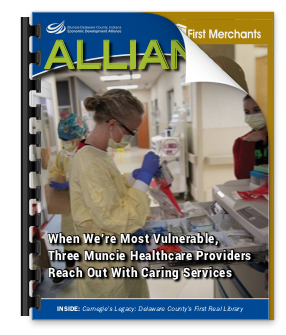
You may view the entire article and view the full Summer 2020 Edition of the Alliance Magazine, by clicking (or tapping on your screen if using a smartphone or tablet) on the magazine’s front cover image below.