By Mike Rhodes, Editor-in-Chief, MuncieJournal.com—
Muncie, IN— A message in my INBOX from the American Heart Association said May is National Stroke Awareness Month. Hashtag #StrokeMonth
How appropriate and timely.
Today is the 2nd anniversary of my stroke.
For what its worth, here’s my story and things you can do to watch for stroke signs in your loved ones. I don’t mind sharing my story because there are lessons to be learned that may help others. In fact, soon after my stroke when I was struggling with “why me” questions, I thought one reason “why me” might be I was supposed to use my communications skills to help others understand stroke better. So, let’s give it a try. I’ve been writing this article a little at a time for the past two years.
In fact, my WordPress dashboard indicates I’ve come back to this page and attempted to add more writing to it a total of 106 times over the last 24 months.
To begin, let’s define what a stroke is: A stroke occurs when the blood supply to part of the brain is suddenly interrupted or when a blood vessel in the brain bursts, spilling blood into the spaces surrounding brain cells. There are two types of stroke: ischemic (clot) or hemorrhagic (bleeding.)
And so it begins…Sunday, May 18, 2020, 7pm
It was a cold and rainy Sunday, deep within the confines of the COVID-19 pandemic that left us with not much to do. And nowhere to go. It was a full day of hanging out on the sofa and Netflix binging. About 7pm that evening I suddenly noticed that the fingertips on my left hand had gone numb and tingly. I thought I might have gotten some kind of weird solution on my hand or something, so I went and washed my hands thoroughly. No difference. The tingly feeling made me stand up and pace around our living room. I asked my wife if she’d go on a short walk with me. During the walk my entire arm started hurting badly…it literally felt like my arm was a wash cloth that was being wrung tighter and tighter and tighter.
“I must be having a heart attack,” I thought. (WRONG!) It was a stroke caused by a carotid artery dissection (tear) in my neck. Here’s the unedited physician notes straight out of my IU Health online medical record:
“60-year-old male patient with longtime smoking history, presented with left sided numbness and tingling from face to arm to leg area (left sided) . Patient started having numbness and tingling on the left side of his body from face to the lower extremity last night. This came on spontaneously. He came to the emergency room because of these symptoms persisted. Pt had recently been tx with antibiotics for pneumonia in March. He felt like he did not have any complete resolution as he continues to have mild shortness of breath as well as continuous dry cough. He denies having fever at home although here in the emergency room he was found to have low-grade fever, no sick contact. Initially he was also found to have a very high blood pressure that already came down to 140/89 at this time. Because of his symptoms several imaging modality patient had were done CT of head and neck showed dissection involving the right distal cervical portion of the internal carotid artery CT head showed mild microvascular ischemic changes and no CT evidence of acute intracranial hemorrhage mass or large territory territorial infarction. His symptoms did improve, and MRI noted: Acute right lateral thalamic / posterior limb of internal capsule
small infarct.”
Anyway, back to my throbbing arm…As I began pondering my medical state it occurred to me that I had no primary care physician any longer. My doctor had left and moved to Fishers a month prior and I had not made arrangements to find another doc for myself. I had nowhere to go except to ER. I didn’t relish waiting around in what might be a long wait in the ER due to COVID, so I waited to go until the following morning. (WRONG!) Should have gone immediately. The key is getting treatment ASAP. I later learned, if you can get to the hospital fast, in some cases, they can give you the drug TPA which can potentially reverse some stroke damage. TPA must be administered within 3 hours of the onset of the stroke. So I really flubbed up on the decision to wait until morning to get to the hospital.
Monday, May 19, 2020, 4:30am
After a sleepless night I got up, showered and told my wife we were going to the hospital. We got to the ER about 5am. Sharon dropped me off at the front door and said she would go park the car and then meet me back in the ER. That was the last I saw of her for four days because the hospital had closed off entry for visitors due to COVID-19. Not having her with me was very disheartening because even though I had worked at Ball Memorial Hospital during my career, I had never been an inpatient. No surgeries. No broken bones. No ER visits. Nothing.
I was scared and I wanted my wife with me. No dice.
I walked up to the ER window with my insurance card extended and announced, “I’ve either had a heart attack or a stroke.” I barely finished my statement when I was whisked off to a treatment room. Lots of doctors, nurses and technicians came in the room, each going about their individual duties. One hooked me up to an EKG. Another gave me a COVID test. (Was negative.) Another went through a battery of questions about my symptoms. As I watched the healthcare workers go about their tasks, I noticed some looked rather serious, so I got a bit nervous. They kept writing things on the glass door at the entrance of my ER room. From my vantage point inside the room, the writing was backwards. I took a picture of the door, then reversed the image on my phone, so I could read it, but I still had no idea what any of it meant.
Soon I was moved to my hospital room as an inpatient. The rest of Monday-Wednesday consisted of a battery of tests including CT scans, MRI’s, and whatnot. A number of months later my neurologist, Dr. Alan J. Schmitt, showed me a scan from one of the MRI images and where the problem area was in my brain. The picture below is that scan. In this particular scan, the MRI had taken an image deep within my brain. To better understand the scan, imagine that I was standing up with a digital camera pointing downward above my head. Now imagine that the camera begins to move in a downward motion, moving slowly and actually entering my head until it gets to the bottom of my forehead area—then stops and snaps a picture at that depth. That’s what the scan shows— A slice of my brain somewhere about 4 inches down inside my brain.
Hospital care was simply the best
The staff at Ball Hospital who worked on me did incredible work. From the ER to Radiology to the Progressive Care floor nurses, hospitalists, physicians and housekeeping—everyone treated me with respect, compassion and professionalism at the absolute worst point in my life. One of the nurses noticed I was quite agitated Tuesday morning. She asked if I smoked and did I need a nicotine patch? I sure did and I loved that she caught on to my needs in that regard. Her intuition saved the day. I also received tremendous support from my wife and Facebook friends across the country during and after my hospital stay. THAT was awesome.
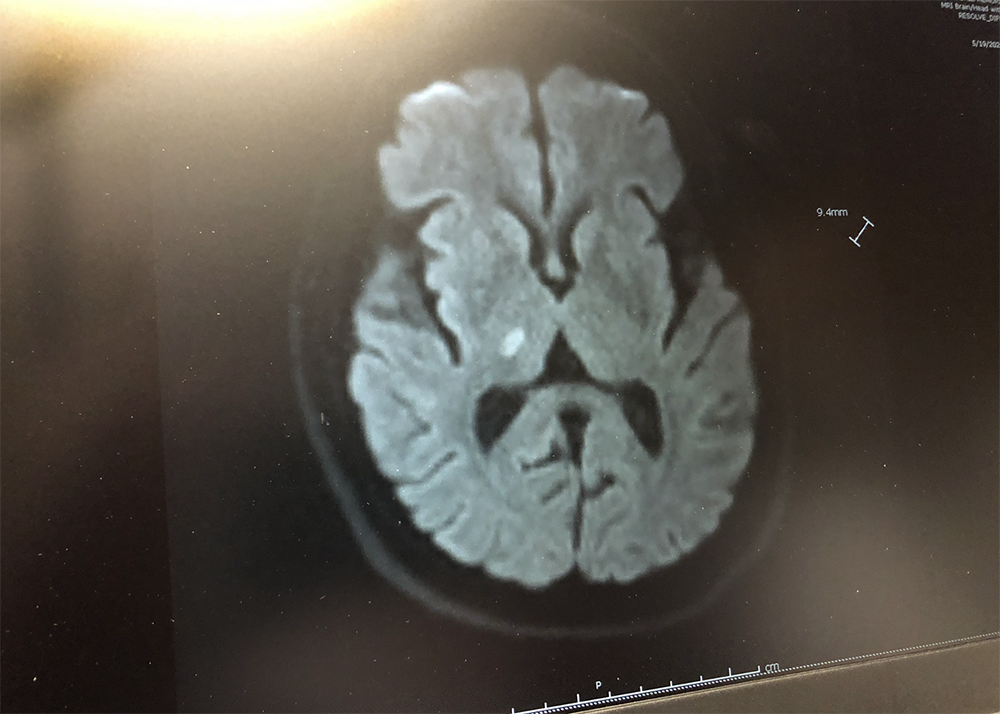
The white area in the center of the picture above is the dead brain area that caused my deficits. Doesn’t really look like all that much, does, it? However, the stroke resulted in my brain becoming chronically confused. It now sends pain messages to my left side, mainly to my arm and hand. The pain messages are constant and chronic. 24/7. It appears that my condition will not change going forward and I will have to live with “how I am now.” The last resort would be brain surgery where an electrical implant would be affixed to the inside of my brain somewhere to stop the pain signals from occurring. No thanks.
Years One and Two and Lessons Learned
First let me say that I am very cognizant of the fact that I was very fortunate that my deficits were not worse than they are. Many, people have seriously debilitating strokes that severely reduced their quality of life. Because of that, many stroke victims are at high risk of becoming suicidal. Compared with the brain scan above, their brains show up as almost totally white, with large patches of white, damaged brain areas.
The stroke I had was MY fault.I smoked cigarettes for a very long time.
I had out-of-control high blood pressure.
I had out-of-control diabetes type 2.
I had out-of-control bad cholesterol.
I stressed over anything and everything. And if there was nothing to stress about, I stressed about having no stress.
All of those bad health habits contributed to my stroke.
For the first year, I slept. A lot. An amazing amount of sleep. Entire weekends were spent sleeping. I found that allowing the brain to rest was normal in the early recovery stage of stroke. Pain was the real issue for me. I could barely ride in a car. Bumps in the road sent pain spikes shooting down my arm and left hand. I had to place my arm on a thick pillow so the pain was reduced enough that I could even stand riding in a vehicle.
I could not tie my shoes. I hated having the outside wind blow across my arm as it caused more pain. I had trouble putting a shirt on. I couldn’t tuck my shirt in. I could not squeeze a tube of toothpaste. I could not swallow very well as the stroke disturbed muscles in my throat. All these little inconveniences one takes for granted caused me daily pain. I could not write, as it caused tremendous pain in my hand. I could not play the piano—a love I’d had most of my life.
My wife thought I needed some cheering up, so she gifted me with a DJI drone. She thought it would be good therapy for my left hand—having to work the controls with my fingers. She was right. It’s good therapy and there’s always a reward at the end—cool pictures and/or video. The drone imagery has become very useful in my MuncieJournal.com work.
I was put on many medications. Some worked. Some didn’t. So. Many. Medications. They give me dry mouth as a side effect, so I end up drinking well over a gallon of water each day. That adds about 8 pounds or more to to my weight every day.
The medications I’m on also wreck my emotions and I often have a hard time controlling them. When I first went back to work I mentioned to one of my colleagues that I was “not the same as the old Mike.” I feel that is still true today. I find some things I used to do easily and well, take an enormous amount of energy and focus to accomplish. My left hand is still very weak. I drop my iPhone all the time and a few weeks ago, I even dropped my Nikon DLSR to the ground. Yikes!
The good news is, today, I am way better than I was two years ago. I have improved in many areas:
I continue to get better movement out of my hand and finger extension.
I stopped smoking and have not had a cigarette since I was in the hospital. 24 months as of today.
My blood pressure is continually in the normal range now. (Just now checked it. It is 126/82.)
I purchased an electronic device that allows me to check my blood sugar with my cell phone, in order to get my blood sugar numbers in better control.
I try to “give less of a care” about things and attempt to keep my emotions in check. That’s important because I still have an aneurysm that could blow at any given time, and getting emotional increases the chance of that happening. The mix of medications makes controlling the emotions difficult.
I can play my synthesizer for a little bit now. It still hurts to play, but it is good therapy for the left hand. I’ve connected it to my Macintosh and have begun creating electronic compositions through the synchronization between my hardware synth and DAW software. THAT combination has made it easier to play, allowing the computer to do some of the work. Click below to listen to what that sounds like.
There are a good number of resources below about #StrokeMonth that you can share in your office or post to your website. The CDC link at the bottom of this page has a great media kit to use however you see fit within your organization. I encourage you take a look at the resources below and share them and this article.
If you’ve read this massive, overly worded page, and wonder what advice I might have on this anniversary day, it’s simply this: Take a deep breath and just enjoy your life.
Stroke Resources
Stroke Resources for Caregivers and Stroke Survivors
Stroke and Aneurysm: What’s the Difference?
Facebook Stroke Survivor Support Group
IU Health/Ball Memorial Hospital Receives Stroke Award
Click the graphic below to get the media kit from the CDC.